Abstract
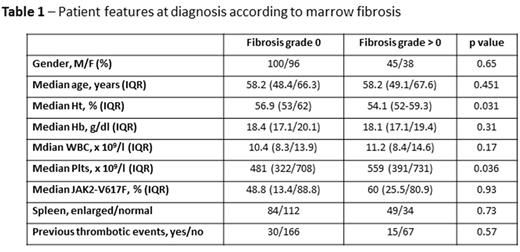
According to the WHO 2016 revised classification of myeloproliferative disorders, bone marrow biopsy is included among the major criteria for the diagnosis of policythemia vera (PV). However, the prognostic role of marrow fibrosis at baseline in PV patients is still controversial and, to date, there are few data in the literature focusing on this issue. We retrospectively analyzed the histologic features at diagnosis of 279 patients affected by PV managed at our Institution from 01/1982 to 05/2014 and with an available bone marrow analysis. Patients' characteristics at diagnosis were: male/female 146/133 (52.3%/47.7%), median age 58.2 years [interquartile range (IQR) 48.8-66.6], median Hb 18.2 g/dl (IQR 17.1-19.7), median WBC 10.5 x 109/l (IQR 8.3-13.9), median PLTs 501 x 109/l (IQR 343-711) and median JAK2-V617F allele burden 57.4% (IQR 18.1-86.1). Furthermore, 115 (41.2%) patients presented an enlarged spleen at diagnosis and 45 (16.1%) reported a thrombotic episode prior to diagnosis. According to the histologic bone marrow findings at diagnosis, 196 (70.2%) patients presented a bone marrow fibrosis grade 0, while 83 (29.7%) had a grade >0 fibrosis (grade I-II). The baseline features of the two subsets of patients were compared (Table 1): a significant difference was observed only with regard to the Ht value (p=0.031) and the PLT value (p=0.036). After a median follow-up of 136 months (IQR 67.5-213.7), the two groups were compared in terms of thrombotic episodes developed during the follow-up [56/279 patients (20%)], evolution into a myelofibrotic phase (MF) [41/279 patients (14.6%)], evolution into a blastic phase (BP) [21/279 patients (7.5%)] and overall survival (OS). The subset of patients with a marrow fibrosis >0 showed a trend towards significance for a reduced occurrence of thrombotic episodes during the follow-up [10/83 (12%) vs 46/196 (23.4%), p=0.096). We did not find any statistical difference between the two groups considering the rate of evolution into MF [9/83 (10.8%) vs 32/196 (16.3%), p=0.23], the rate of evolution into BP [4/83 (4.8%) vs 17/196 (6%), p=0.23) and the median OS (110.7 vs 113.5 months, p=0.771). According to our data, the presence of a bone marrow fibrosis at baseline in PV patients was associated only to a trend towards a decreased risk of developing thrombotic events and did not influence the follow-up and prognosis. Taken together, these data do not confirm the prognostic impact of bone marrow fibrosis in PV and suggest that further prospective evaluations are warranted to conclusively clarify this controversial issue.
Breccia: Pfizer: Consultancy; Bristol Myers Squibb: Consultancy; Incyte: Consultancy; Novartis: Consultancy. Foa: Sandoz: Consultancy, Speakers Bureau; Novartis: Consultancy, Speakers Bureau; Amgen: Consultancy, Speakers Bureau; Celgene: Consultancy, Speakers Bureau; Gilead: Consultancy, Speakers Bureau; BMS: Consultancy, Speakers Bureau; Janssen: Consultancy, Speakers Bureau; Roche: Consultancy, Speakers Bureau; Abbvie: Consultancy, Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal